BOISE, Idaho — Idaho is reporting 1,830 new cases of COVID-19, the fourth highest daily caseload, along with 13 new deaths Tuesday. The big focus is on hospital capacity after medical leaders enacted crisis standards of care on Sept. 16. They are still in effect.
As of Friday, more than 670 people were in the hospital with COVID. That's a drop from our all-time record of 717, which was set last Thursday. Meantime, ICU cases rose to 192, which is a new record.
The Idaho Department of Health and Welfare held another COVID-19 media briefing Tuesday. It was streamed live on KTVB.COM on our YouTube channel.
Health and Welfare Director Dave Jeppesen opened the briefing by saying the surge of COVID-19 cases has exceeded the health care resources that are available. However, this does not mean that hospitals will be universally applying do not resuscitate orders.
Jeppesen said his family has already seen firsthand the difference in the level of care that crisis standards of care brings to Idaho hospitals. On Thursday, Sept. 16, the same day that crisis standards of care was activated across the state, Jeppesen's mother had a stroke and was taken to St. Luke's in Boise for treatment.
"Things were different in the ER," Jeppesen said. "There were other patients receiving care in the waiting room. My mom fell when she had her stroke and there was a concern that she had broken bones. The X-rays were done in a non-traditional X-ray area with a longer wait than usual. Fortunately, she did not break any bones. Normally a person in her condition would be held overnight for observation. Because of crisis standards of care, after she was stable, she was discharged later the same day from the ER."
Jeppesen said his mother is now recovering at home and is the care of his family. He praised the health care professionals at St. Luke's and said those same dedicated health care professionals across the state need our help. We need the unvaccinated to get the COVID-19 vaccine, he said.
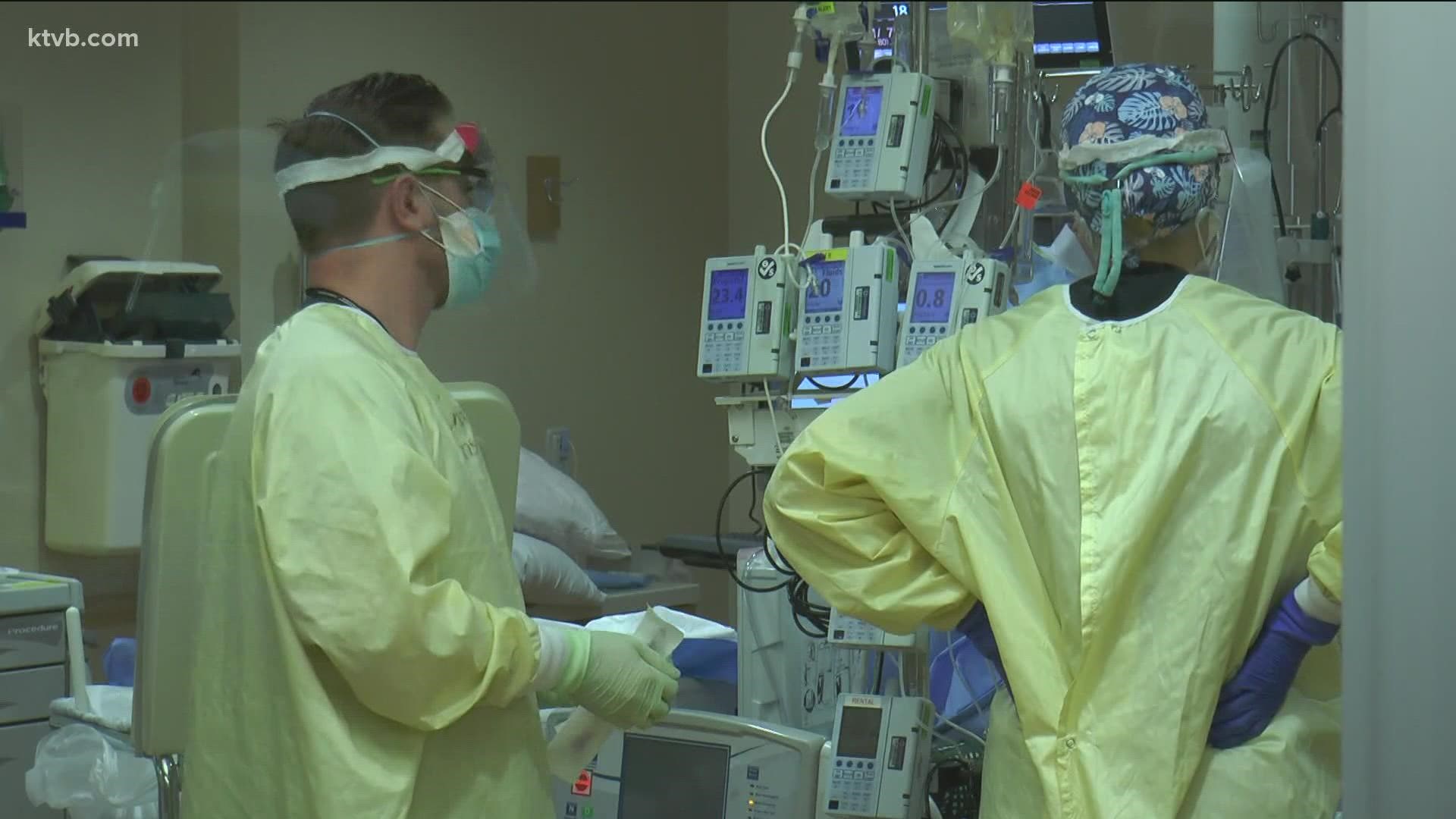
Dr. Jim Souza, chief physician executive at St. Luke's Health System in Boise, was on the call Tuesday. He said their facilities are progressively becoming "COVID hospitals."
"We've gone from 33 COVID hospitalizations in our system in July to 289 today, that's at St. Luke's," Souza said. "COVID previously accounted for about 8% of our adult hospitalizations and today it accounts for 67% with this single diagnosis. That's an unprecedented event in modern medicine."
The news is a bit worse when you look inside their intensive care units. In July, there were eight COVID patients in the ICU at St. Luke's, making up around 17% of all ICU patients. Today, that number stands at 51, or 70% of patients.
Souza outlined five important differences they are seeing in COVID patients now as opposed to the ones they saw last December. First, they are much younger. The average age has gone from 72 to 58. There are 36 COVID patients in the ICU under 55 and 13 under the age of 40. Souza believes that's due to higher number of non-vaccinated patients in the younger population.
"What's new since the introduction of the vaccines is that we are mostly not seeing an entire segment of the population in our hospitals - the vaccinated," Souza said. "We're not seeing them. And we almost never see those individuals in our intensive care units."
Third, patients are more sick, and most are on ventilators. Fourth, the length of stay in the ICU, if they survive, is longer. The average stay is around eight days. And finally, these patients are dying more frequently. The mortality rate among COVID patients in the ICU has climbed from 28% to 43%.
"We've had 80 deaths from COVID in our health system since the beginning of September," Souza said. "That's four every day the sun comes up. 35 of those occurred in the last week."
He says if you look at all the ages of the people who died in September, and figure it in terms of average life spans, it's a tragic loss of life.
"It's more than 1,100 life years. A life year is one person's experienced year of life. Can you imagine?" Dr. Souza said. "And for the people who say we all die some time, yes we do. But these people didn't need to die now, and they didn't need to die like this."
He goes on to say, for those who go to the ICU and survive, they will be terribly disabled for months.
When it comes to monoclonal antibodies, state epidemiologist Dr. Christine Hahn revealed the treatment center in northern Idaho treated 90 patients in its first three days.
Experts say, getting the treatment only works if you get COVID or if you're immunocompromised and you're exposed to COVID. It's not a replacement for the vaccine, but because of an increased demand, there will now be a reduction in the number of antibodies allocated to the state, which means, the state could potentially later look at who is eligible and prioritize, but they have not done that yet. If you want to find a provider near you, click here.
You can watch the full COVID-19-briefing below: