BOISE, Idaho — Hospitals in Idaho have not instituted an across-the-board practice to stop giving CPR to patients on the brink of death, officials say, despite an outline for crisis care standards that would allow that if the state's fight against COVID-19 grows more desperate.
At issue is a medical order known as a "do not resuscitate" order, or DNR. The medical decision, which doctors issue at the request of a patient or patient's family, instructs healthcare workers not to provide chest compressions, mouth-to-mouth breathing, intubation, or an electrical shock to restart a heart's normal rhythm in the event the person's heart stops.
Typically considered by the terminally ill and very elderly, a DNR allows a patient in end-of-life care to die without intervention.
On Thursday, crisis standards of care were expanded across the state in response to a wave of serious COVID-19 infections overwhelming hospitals' ability to care for all the sick. Under crisis standards, hospitals are tasked with providing care to and keeping alive as many people as possible. The standards allow healthcare workers to ration beds, medicine, ventilators, and other resources to those deemed most likely to survive their illness or injury.
In an Idaho Department of Health and Welfare document on strategies for patient care in "scarce resource situations," the Crisis Standards of Care Activation Advisory Committee opened the door to allow a universal DNR order for every adult patient who is brought in to a hospital.
The universal DNR can only be used during a public health emergency, when crisis standards have been declared, and when the demand for ventilators have exceeded a hospital's supply.
In such a circumstance, an adult patient "should receive NO attempts at resuscitation (compressions, shocks or intubation if not yet intubated) in the event of cardiac arrest," the document reads.
Pediatric patients would not be included under such a blanket DNR.
"The likelihood of survival after a cardiac arrest is extremely low for adult patients," the standards read. "As well, resuscitation poses significant risk to healthcare workers due to aerosolization of body fluids and uses large quantities of scarce resources such as staff time, personal protective equipment, and lifesaving medications, with minimal opportunity for benefit."
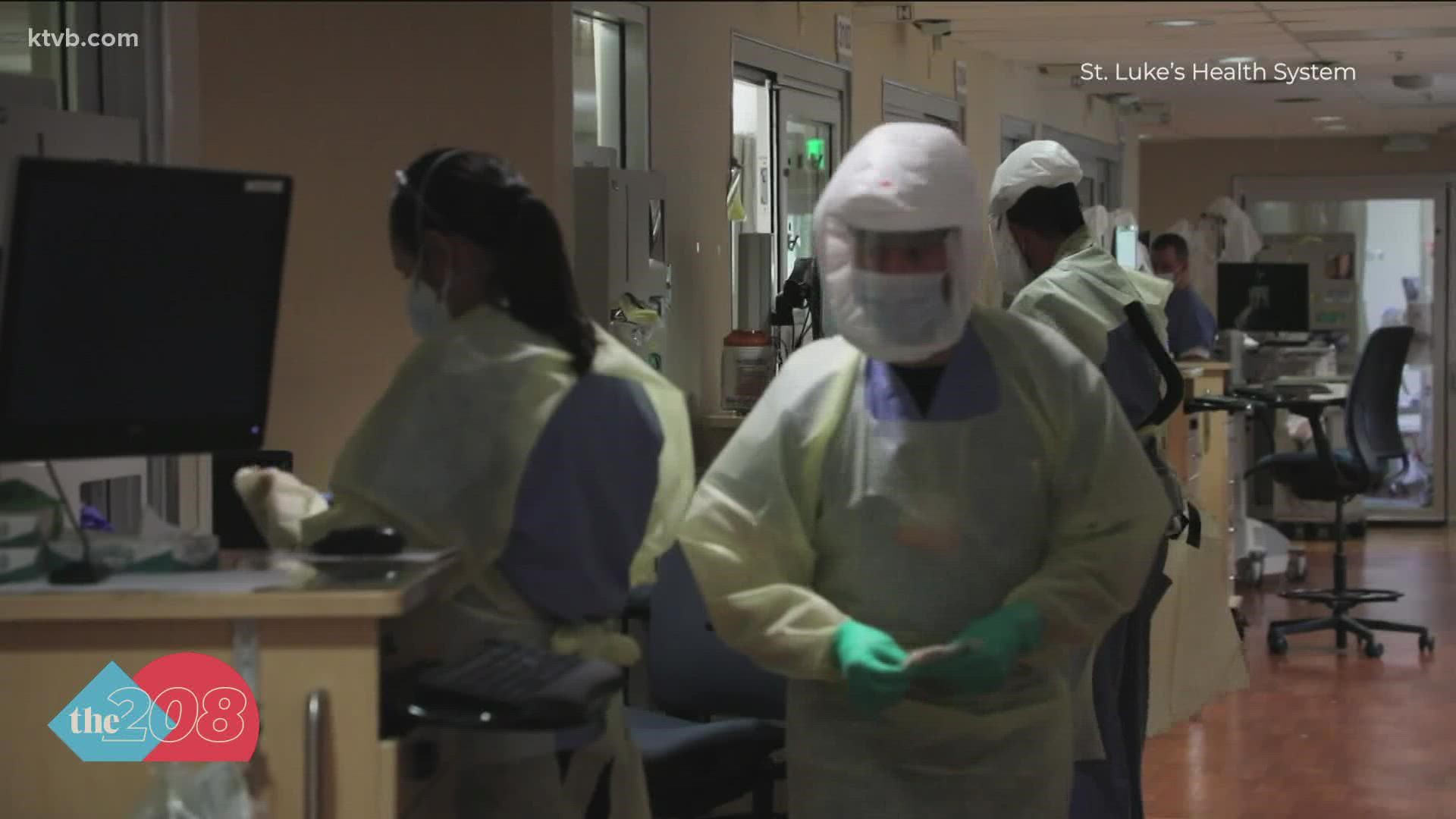
But Jim Souza, Chief Physician Executive for St. Luke's, says neither his hospital nor any other in Idaho has instituted a blanket DNR order on their patients' behalf.
The Health and Welfare documents provide guidelines for healthcare facilities to make the grueling decisions that are necessary when medical need outstrips what a hospital can provide.
Souza said hospitals can decide what from those guidelines to put into practice.
"Each individual facility is expected to create its own implementation plan, and to my knowledge, no healthcare facilities in the state endorse that," he said of the universal do not resuscitate proposal. "That certainly includes St Luke's, and I know I can speak for Saint Alphonsus as well."
Putting a DNR in place is a decision made with those who are ill and their families, Souza said.
"We speak with patients and their families about their preferences, you know, do they want us to attempt to [do] resuscitation?" he said. "We certainly have patients and families who say 'yeah, don't do that.' And when we hear that, we respect and honor that request, but there's no blanket order to not resuscitate people at all."
At KTVB, we’re focusing our news coverage on the facts and not the fear around the virus. To see our full coverage, visit our coronavirus section, here: www.ktvb.com/coronavirus.
Facts not fear: More on coronavirus
See our latest updates in our YouTube playlist: